Just how gnarrowh are the ACA networks – and how much do the insured care?
Joanne Kenen
March 14, 2016 - Association of Health Care Journalists
We all hear stories (and perhaps have personal experience) of people having trouble accessing one of their regular physicians or having trouble getting a desired specialist because of gnarrow networksh that offer a more limited choice of doctors and hospitals.
In some states, such as Texas, there has been a significant shift in the individual market to narrow network plans, and away from preferred provider organizations (PPOs) and similar networks providing broader choice and more out of network options.
Criticism of limiting choice has been a common line of attack by the critics of the Affordable Care Act. President Obama did, after all, promise that Americans could gkeep their doctorh – an oversimplification for which he paid a political price.
Two recent studies bear looking at. One from the Robert Wood Johnson Foundation (summary and full issue brief) found that most highly-ranked hospitals do participate in one or more exchange plans – though they may limit the number of plans they contract with. A second survey, from the Kaiser Family Foundation, suggests that most people donft really object to narrow networks if it saves them money. (This isnft the only study of its kind, but itfs recent).
The RWJF survey has limits because data isnft available on all provider networks. The study relied on those deemed gbest regional hospitalsh by U.S. News and World Report. It found that gnearly all of the highly ranked hospitals were in-network with at least one marketplace plan in both 2015 and 2016. The percent participating stayed nearly the same, at the very high rate of 97 percent in 2015 and 96 percent in 2016.h
However, the hospitals did participate in fewer networks:
gLooking at changes in participation, only 43 percent of these hospitals maintained or increased the number of marketplace networks in which they participated, while 57 percent of hospitals participated in fewer networks in 2016. Nationally, the number of marketplace networks that included a regionally ranked hospital declined by 20 percent, from 597 to 476.h
Thatfs a decline worth paying attention to – and we need to watch for decline next year. But itfs still a lot higher participation than a lot of the conventional wisdom, or conventional criticism, would make one expect. (Therefs also state-to-state variation – worth looking at how your state is faring – see the detailed data starting page 4 of the issue brief). And while the number of hospitals taking part in two or three exchange plans was pretty stable, the number doing four did drop.
The second finding from Kaiser was part of the foundationfs monthly tracking poll – and you need to scroll down past the election season analysis to get to the narrow network findings. But here it is:
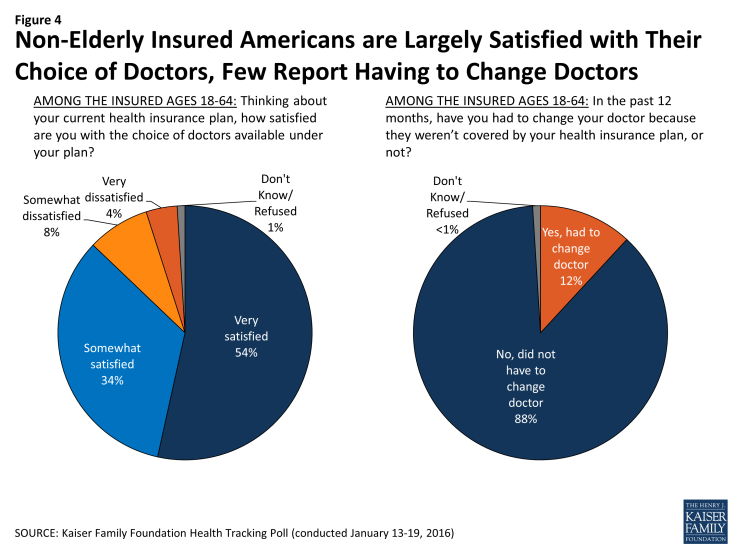
gThose with insurance are largely satisfied with the choice of doctors available under their plan. Nearly 9 in 10 (87 percent) of the non-elderly [not Medicare age] insured say they are everyf or esomewhatf satisfied, while just 12 percent say they are everyf or esomewhatf dissatisfied. Just 12 percent of the non-elderly insured say they have had to change doctors in the past 12 months because their doctor wasnft covered by their health insurance plan, including 5 percent who say the change was a big problem for them, 5 percent who say it was a small problem and 1 percent who say it was not a problem.h